Introduction to Specimen Collection
Laboratory tests contribute vital information about a patient's health. Correct diagnostic and therapeutic decisions rely, in part, on the accuracy of test results. Adequate patient preparation, specimen collection, and specimen handling are essential prerequisites for accurate test results. The accuracy of test results is dependent on the integrity of specimens.
Safety and Disposal Considerations in Specimen Collection
In all settings in which specimens are collected and prepared for testing, laboratory and health care personnel should follow current recommended sterile techniques, including precautions regarding the use of needles and other sterile equipment. Treat all biological material as material that is potentially hazardous as well as contaminated specimen collection supplies. For all those who are involved in specimen collection and preparation, the responsibility to adhere to current recommendations designed to maintain the safety of both patients and health care workers does not end when the patient is dismissed.
There are four steps involved in obtaining a good quality specimen for testing: (1) preparation of the patient, (2) collection of the specimen, (3) processing the specimen, and (4) storing and/or transporting the specimen. Since information related to any of these areas may change as clinical laboratory technology changes, please refer to the latest edition of the Labcorp Directory of Services and Interpretive Guide for current instructions.
Preparation
Prior to each collection, review the appropriate test description, including the specimen type indicated, the volume, the procedure, the collection materials, patient preparation, and storage and handling instructions.
Preparing the Patient. Provide the patient, in advance, with appropriate collection instructions and information on fasting, diet, and medication restrictions when indicated for the specific test.
Preparing the Specimen. Verify the patient's identification. Proper identification of specimens is extremely important. All primary specimen containers must be labeled with at least two identifiers at the time of collection. Submitted slides may be labeled with a single identifier, but two identifiers are preferred. Examples of acceptable identifiers include (but are not limited to): patient's name (patient's first and last name exactly as they appear on the test request form), date of birth, hospital number, test request form number, accession number, or unique random number. A
location such as a hospital room number is not an appropriate patient identifier. If chain of custody documentation is necessary for the procedure, follow the appropriate protocol. All specimens should be labeled in the presence of the patient. Process and store the specimen(s) as required. Appropriate storage and handling are necessary to maintain the integrity of the specimen and, consequently, the test results.
Avoiding Common Problems
Careful attention to routine procedures can eliminate most of the potential problems related to specimen collection. Materials provided by the laboratory for specimen collection can maintain the quality of the specimen only when they are used in strict accordance with the instructions provided. To collect a sufficient quantity of each type of specimen indicated for the procedures to be performed, please consult the volume requirements published in this Directory.
General Specimen Collection. Some of the common considerations affecting all types of specimens:
- Please examine specimen collection and transportation supplies to be sure they do not include expired containers.
- Label a specimen correctly and provide all pertinent information required on the test request form. (See Blood Specimens: Chemistry and Hematology − Blood Collection/Transport Containers.)
- Submit a quantity of specimen sufficient to perform the test and avoid a QNS (quantity not sufficient), as indicated in the test requirements. (See Quantity Not Sufficient.)
- Use the container/tube indicated in the test requirements for appropriate specimen preservation.
- Follow patient instructions prior to specimen collection Including the proper order of blood draw when multiple tubes are required. (See Blood Specimens: Chemistry and Hematology – Consideration for Single and Multiple Sample Collection.)
- Carefully tighten specimen container lids to avoid leakage and/or potential contamination of specimens.
- Maintain and transport the specimen at the temperature indicated in the test requirements.
- Mix specimen with additive immediately after collection by inverting 5-10 times.
Serum Preparation. The most common serum preparation considerations:
- Separate serum from red cells within two hours of venipuncture.
- Mix by inverting specimen with additive immediately after collection.
- Allow specimens collected in a clot tube (eg, red-top or gel-barrier tube) to clot before centrifugation. (See Blood Specimens: Chemistry and Hematology − Preparing Serum on clotting and gel-barrier tubes and red-top tubes.)
- Avoid hemolysis: red blood cells broken down and components spilled into serum. Causes and prevention are discussed under the section on hemolysis.
- Avoid lipemia: cloudy or milky serum sometimes due to the patient's diet (discussed under the section on lipemia).
Plasma Preparation. The most common considerations in the preparation of plasma:
- Collect specimen in additive indicated in the test requirements.
- Mix specimen with additive immediately after collection by inverting 5-10 times.
- Avoid hemolysis or red blood cell breakdown.
- Fill the tube completely, thereby avoiding a dilution factor excessive for total specimen volume (QNS).
- Separate plasma from cells within two hours of venipuncture or as indicated in the test requirements.
- Label transport tubes as “plasma”
- Indicate type of anticoagulant (eg, “EDTA,” “citrate,” etc)
Urine Collection. The most common urine collection considerations:
- Obtain a clean-catch, midstream specimen.
- Store unpreserved specimens refrigerated or in a cool place until ready for transport.
- Provide patients with instructions for 24-hour urine collection(s).
- Add the preservative (as specified in the test requirements) to the urine collection container prior to collection of the specimen if the preservative is not already in the container.
- Provide sufficient quantity of specimen to meet the minimum fill line on preservative transport container.
- Provide the proper mixing of specimen with urine preservative as specified in the test requirements.
- Use the collection container as specified in the test requirements, and refrigerate the specimen when bacteriological examination of the specimen is required.
- Carefully tighten specimen container lids to avoid leakage of specimen.
- Divide specimen into separate containers for tests with such requirements.
- Provide a complete 24-hour collection/aliquot or other timed specimen.
- Provide a 24-hour urine volume when an aliquot from the 24-hour collection is submitted.
- Preservatives vary for each test; refer to test information for the required preservative.
Collection Procedures
Collection of Vacuum Tubes Containing Additives (eg, anticoagulants, preservatives, clot activators, gel-barrier). When using vacuum tubes containing an additive:
- Tap the tube gently at a point just below the top to release any additive adhering to the tube or top.
- Permit the tube to fill completely to ensure the proper ratio of blood to additive. There will be some dead space at the top of the tube.
- To allow for adequate mixing of blood with the anticoagulant or preservative, use a slow rolling wrist motion to invert the tube gently four to eight times. Failure to invert tubes may lead to the formation of microscopic clots.
- Rapid wrist motion or vigorous shaking may contribute to hemolysis.
- Check to see that all the preservative or anticoagulant is dissolved. If any preservative powder is visible, continue inverting the tube slowly until the powder is dissolved.
- If multiple samples are being drawn, invert each specimen as soon as it is drawn. Do not delay. Place the tube upright in a rack as quickly as possible after collection.
- The gel-barrier tube is an additive tube and should be inverted five to six times after collection. Allow the tube to stand for 30 to 60 minutes for complete clotting to occur prior to centrifugation.
Collection of Vacuum Tubes Without Anticoagulants. When using vacuum tubes containing no additives:
- Permit the tube to fill completely.
- Let the specimen stand for 30 to 60 minutes and (preferably) not longer than 60 minutes prior to centrifugation.
- Centrifuge the specimen at the end of the waiting period in accordance with the manufacturer's instructions for speed.
Hemolysis
In general, grossly or even moderately hemolyzed blood specimens may not be acceptable for testing. Hemolysis occurs when the red cells rupture and hemoglobin and other intracellular components spill into the serum. Hemolyzed serum or plasma is pink or red, rather than the normal clear straw or pale yellow color.
Most cases of hemolysis can be avoided by observing the steps listed.
- For routine collections, use a 21- to 22-gauge needle. (On occasion, however, it may be necessary to use a 23-gauge needle for patients from elderly and pediatric populations with small or difficult veins.)
- If there is air leakage around the needle or loss of vacuum in the tube, replace the vacuum tube.
- If you are using your own collection equipment instead of the vacuum tube technique, use only clean, dry, sterile needles, syringes, and tubes.
- Collect blood in room temperature containers unless the specimen requirement specifies otherwise.
- When there is difficulty accessing a vein or when a vacuum tube fills too slowly due to a difficult venipuncture, damage to the red blood cells may result. Address this problem by collecting a fresh tube when blood flow is established or select another puncture site and, using sterile/unused equipment, collect a second specimen. Also, use of a blood pressure cuff, in lieu of a tourniquet, will reduce trauma to fragile red blood cells.
- Do not remove the needle from the vein with the vacuum tube engaged. This applies to both the last tube collected during a routine venipuncture and to tubes collected during a difficult procedure.
- Premature removal of the tube causes a rush of air to enter the tube, which may result in damage to the red cells.
- Be as gentle as possible, drawing the blood evenly. Too much pressure in drawing blood into a syringe or forcefully ejecting blood into a collection tube from a syringe may damage red cells.
- Allow collection site to dry after cleaning with the alcohol pad. Alcohol used to clean the puncture site may cause contamination in a tube.
- Do not collect a specimen from or through a hematoma.
- Allow specimen to clot completely (for 30 to 60 minutes) before centrifuging.
- Do not centrifuge the specimen for more than 10 minutes unless otherwise specified by the collection instructions.
Lipemic Serum or Plasma (Turbidity)
Normal serum or plasma is a clear and light yellow to straw in color. Turbid serum or plasma appears cloudy or milky.
Serum or plasma may be cloudy due to bacterial contamination or chronic or transient high lipid levels in the patient's blood.
The primary dietary sources of lipids (fatty substances) are meats, butter, cream, and cheese. Patients who consume these foods within the 24-hour period immediately preceding collection of a blood specimen may have temporarily elevated lipid levels, which may be manifested by cloudy or lipemic serum. Lipemic serum or plasma may not be a true indicator of the patient's physiologic state. (See Figure 1.) Regardless of diet and length of fast, some patients may produce cloudy specimens.

To avoid dietary-induced high lipid levels prior to testing, many physicians require patients to exclude the high-fat foods from their diets or to fast for 12 to 14 hours prior to specimen collection. For morning specimen collection, the laboratory recommends that the patient be required to fast from 6 PM on the previous evening.
Quantity Not Sufficient
One of the most common problems in specimen collection is the submission of an insufficient volume of specimen for testing. The laboratory sends out a report marked QNS (quantity not sufficient), and the patient has to be called back for a repeat collection at an inconvenience to the patient and to the physician. To ensure an adequate specimen volume:
- Always draw whole blood in an amount 2½ times the required volume of serum required for a particular test.
- For example, if 2 mL serum are required, draw at least 5 mL whole blood. If there is difficulty in performing venipuncture, minimum volume may be submitted if it is indicated in the test description. For most profile testing, draw at least two 8.5-mL gel-barrier tubes.
- If pediatric tubes are used, be sure to collect an adequate volume of specimen to perform the test.
- Provide patients with adequate containers and instructions for 24-hour urine and stool collections.
- It is critical, especially for any specimen collection tube containing an additive, to allow the tube to fill to the "fill line" marked on the tube. This requirement is important in order to achieve the proper blood-to-additive ratio; otherwise, the specimen may be found to be QNS.
Specimen Storage and Shipping Temperatures
The definition of specimen temperatures for storage and shipping is as listed below:
Room Temperature: 10.1 – 40.0 oC
Refrigerated: 1.0 to 10.0 oC
Frozen: -1.0 to -80.0 oC
Frozen Specimen Guide
Outdoor Specimen Lockboxes
For clients whose specimen lockboxes must be placed outdoors, adding a frozen gel pack to the lockbox during warmer weather will help provide a moderate temperature inside the lockbox until specimens are collected by your Labcorp service representative. Labcorp also offers a different lockbox for use at locations that experience “extreme” temperatures. Contact your local representative for more information.
Refrigerant Bottles should be prepared for use by placing them in a freezer for four hours or longer. They should be frozen solid prior to being placed in the lockbox, and they should be frozen solid before each use, even though they may be used with specimens that are not frozen.
Number of Frozen Gel Packs Recommended
| Approximate Outdoor Temperature | Frozen Refrigerant Bottles Recommended |
|---|---|
| Below 80°F | None |
| 80°F − 100°F | One Refrigerant Bottle |
| 105°F − 120°F | Two Refrigerant Bottles |
If it is not possible to avoid placing the specimen lockbox in direct sunlight, add 20°F to the temperatures listed above to determine how many frozen gel packs to use. For lockbox instructions and Q&A, select Instructions for Use.
If a specimen that is frozen needs to be put into the lockbox, the Frozen Specimen Keeper can be used maintain that frozen state. Instructions for Use.
Preparing the Patient
Patient Instructions
It is important to gain the patient's understanding and cooperation in obtaining an acceptable specimen.
Patient States
Basal State. In general, specimens for determining the concentration of body constituents should be collected when the patient is in a basal state (ie, in the early morning after awakening and about 12 to 14 hours after the last ingestion of food). Reference intervals are most frequently based on specimens from this collection period.
The composition of blood is altered after meals by nutrients being absorbed into the bloodstream. Consequently, postprandial blood (blood drawn after a meal) is not suitable for some chemistry tests. An overnight fast is preferable (from 6 PM of the evening previous to collection) to ensure that the patient is in the basal state. This minimizes the effects of ingested substances on the test results. Before you collect
the specimen, ask the patient when he/she last ate or drank anything. If the patient has eaten recently and the physician wants the test to be performed anyway, you should indicate “nonfasting” on the test request form. In the clinical information/comments section of the test request form, indicate the time the patient ate. Fasting does not include abstaining from coffee, tea, or sugar-free liquids.
Fasting or diet restrictions, such as low-fat diets, should be explained in detail, particularly to aged or overanxious patients or their caregivers. Inform patients that fasting does not include abstaining from water. Dehydration resulting from water abstinence can alter test results.
When specimens are not collected in the basal state, the following additional effects should be considered when interpreting test results.
- Exercise. Moderate exercise can cause an increase in blood glucose, lactic acid, serum proteins, and creatine kinase (CK).
- Emotional or Physical Stress. The clinical status of the patient can cause variations in test results.
- Time of Day of Collection. Diurnal variations and variations in circadian rhythm can also affect test results. For example, growth hormone peaks in the morning before waking and decreases throughout the day. Serum iron levels may change as much as 30% to 50%, depending on individual variation, from morning until evening.
Note: For chemistry profiles, 12- to 14-hour fasting specimens are recommended.
Timed Specimens
There are two types of timed blood specimens: One is for a single blood specimen ordered to be drawn at a specific time. The other is for a test that may require multiple blood specimens to be collected at several specific times.
Single Specimens. Here are some instances in which timed single specimens may be required.
- Fasting plasma glucose alone or in conjunction with a random glucose determination, as recommended by the American Diabetes Association, to diagnose diabetes. Fasting here is defined as no caloric intake for at least eight hours.
- Postprandial glucose may be performed two hours after a meal for a timed test that is helpful in diabetes detection.
- Blood glucose determinations may be ordered at a specific time to check the effect of insulin treatment.
- Blood cultures may be ordered for a specific time if a bloodstream bacterial infection is suspected.
- Therapeutic monitoring of patients on medication.
Multiple Specimens. Here are some instances in which timed multiple specimen tests may be ordered
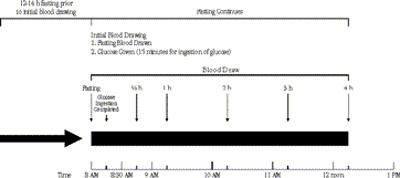
- The most common timed procedure is a glucose tolerance test. First, a blood specimen is drawn from a fasting patient. Then, the patient is given glucose orally and blood specimens are drawn at fixed intervals. (See following illustration.) Note: The American Diabetes Association and the World Health Organization (WHO) have specific recommendations for glucose tolerance testing.
- The tolbutamide (Orinase®) test is similar to a glucose tolerance test, but the collection intervals vary.
- To test the effect of a certain medication, a physician may order the same test to be obtained on consecutive days, before, during, and after the patient has received a medication.
- Collection of an acute and convalescent serum to aid in the diagnosis of a viral infection when culturing is not feasible.
- Other examples include such tests as occult blood, ova and parasites, and blood cultures.
Sequential Sampling
Diagnosis of many endocrine diseases requires sequential sampling of blood and/or urine. Labcorp sometimes offers reduced fees for serial tests when the following conditions are met:
- All sequential specimens are from the same patient and are sent to the laboratory at the same time.
- The specimens are clearly labeled with their chronological sequence (1 of 6, 2 of 6, time of drawn or Fasting, ½ hr, 1hr, etc) and with the patient's name, other unique identifier, and date of collection.
- Only one test request form accompanies the serial samples, and it is completed with all patient information, including any medications administered and the number of samples sent.
- The test request form and all specimens are sent in one container (box or plastic specimen transport bag).
Serial Monitoring
Monitoring a patient over time for a specific condition is a variation of sequential sampling. Many tumor markers (tests used to follow the patient's response to treatment for cancer) may be monitored over the course of several years. Specific instructions for serial monitoring are found in the test description for the applicable test being monitored.
Interference of Medications and Other Substances
Many common prescription and nonprescription (over-the-counter) medications can interfere with chemical determinations or alter levels of substances measured. Drug interference is complicated and often method-dependent such that only general recommendations can be stated here. Precautions to be observed must be determined by the physician, and the patient must then be told to avoid specified medications for the necessary periods of time prior to specimen collection.
If the patient cannot be taken off the medication in question, its presence should be noted on the test request form.
Summary: Interference of Medications and Other Substances
- Drugs or their metabolites are frequently concentrated in the urine in sufficient amounts to interfere significantly with urine assays. (See appendices or individual tests for specific information.)
- Drug interference of notable clinical significance has been well-documented in the following instances.
- Thiazide diuretic therapy. The pharmacologic or toxic effect is hyperuricemia and hyperglycemia.
- Catecholamine assay. If a “24-hour drug abstinence period” for a patient is not possible, order VMA or metanephrines.
- Oral contraceptives cause a decrease in serum vitamin B12 levels that is often indistinguishable from vitamin B12 deficiency of any cause. They also cause an increase in total serum thyroxine-binding globulin. This results in increase in both total serum thyroxine and unsaturated thyroxine-binding globulin, but with no significant change in unbound (free) thyroxine.
- Many medications have been shown to have long-term residual effects that interfere with testing. (Biotin is one example of this that is often administered in high dosages.)
- Refer to individual test descriptions for specific information.
